What to do when you receive an unexpected medical bill?
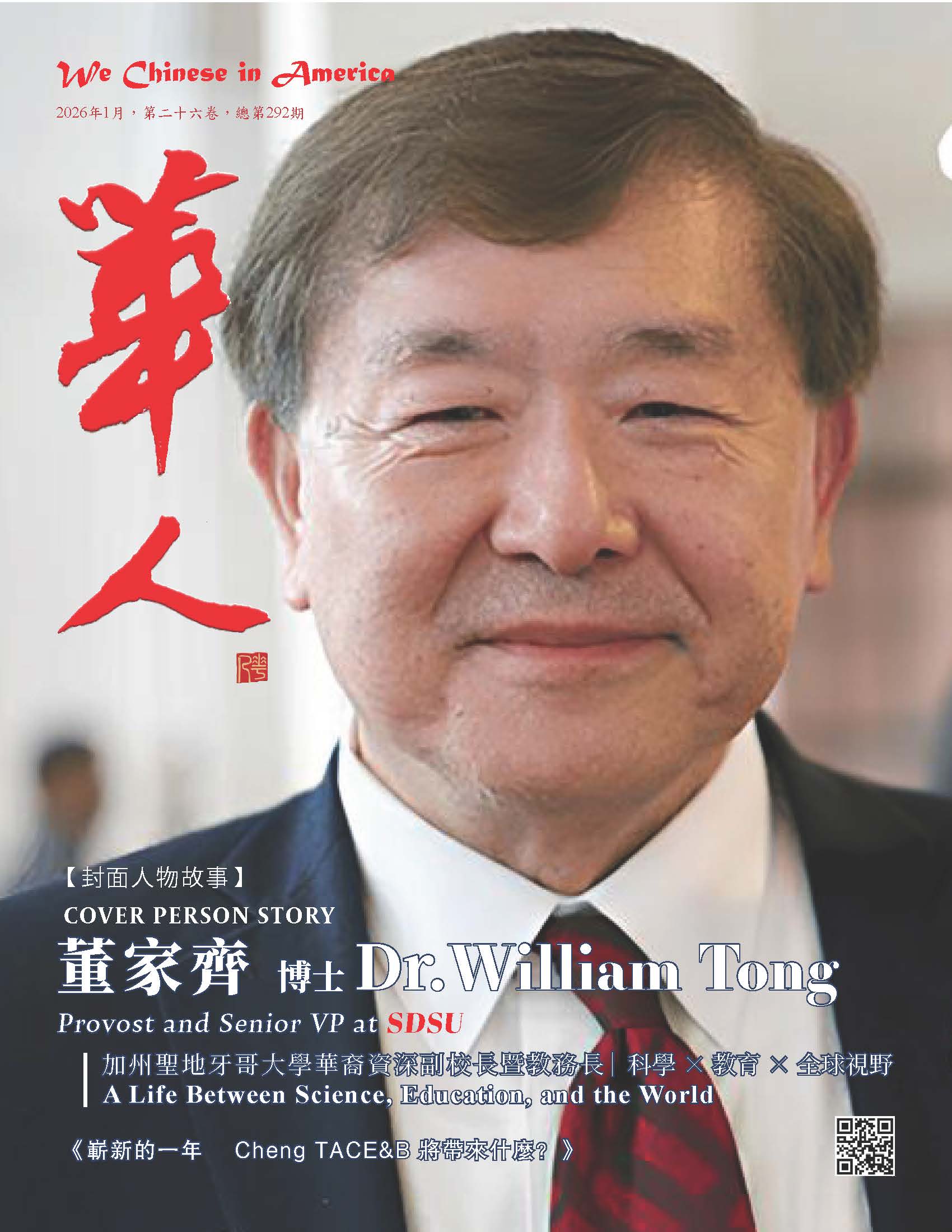
【《We Chinese in America》Media Editor Tang Zhao, July 11, 2022】The "No Surprises Billing Act", which aims to protect consumers' rights and avoid receiving unexpected medical bills after medical treatment, was finally implemented on January 1, 2022. However, consumers may still receive unexpected medical bills, according to an analysis by Consumer Reports. (Unexpected Medical Bill Image from Progressusrevenue.com)
The No Surprises Billing Act is on the way, intending to solve a problem that has plagued millions of Americans for years. In emergencies, consumers often receive unexpectedly expensive medical bills when they use medical services that are not covered by the insurance company, visit a hospital or clinic that is not covered by the insurance company, or involuntarily receive medical care from doctors outside the insurance company system. Surprise medical bills can run into thousands of dollars.
After the introduction of the new law, consumers will be protected by law. To use medical services outside the insurance company's system, you only need to pay the deductible according to the charging standards in the insurance company's system.
★A lot of gray areas
However, the No Surprises Billing Act does not cover medical services that some consumers may need, and certain "gray areas" remain to be clarified.
Chuck Bell, a senior policy analyst at Consumer Reports, said the new law is a landmark victory for people with health insurance. "For the first time in history, patients in all 50 states are protected from having to worry about unexpected medical bills due to emergencies or scheduled elective surgeries," he said.
According to an analysis by the Kaiser Family Foundation, a nonprofit research group, the new law could avoid up to 10 million unexpected medical bills a year, according to federal statistics, but the new law does not protect everyone and every situation.
For example, physicians in insurance systems requiring patients to undergo certain tests are not covered by the new law, and the new law does not apply to certain types of emergency care centers or outpatient clinics, production centers, nursing homes or addiction treatment centers. If people need to take an ambulance for emergency medical treatment, it may not be covered by the new law.
Patricia Kelmar, a health policy advocate at the U.S. Public Research Interest Group (U.S. PIRG), a consumer advocacy group, said these expensive unexpected medical bills can be a source of stress for the public.
With only a few exceptions, people who get health insurance through their employers or self-enroll in the Affordable Care Act (commonly known as Okee) insurance plan are covered by the new law. However, people who use "short-term health insurance" with a validity period of less than 365 days are not covered.
People with Medicare (commonly known as red and blue cards), Medicaid (commonly known as white cards), veterans insurance or active-duty military insurance are not affected by the new law, because the provisions of these federal programs already put in place protections against unexpected medical bills.
Consumer Reports points out that people can still fight for their rights if they receive an unexpected medical bill if:
- ●Emergency Care Outpatient Center
Some EMS outpatient centers are really just general physician offices that cannot handle life-threatening major injuries, some have facilities to deal with breathing difficulties, chest tightness, etc., and others may be licensed by the state to provide emergency medical services.
Jack Hoadley, a professor emeritus at Georgetown University's Health Policy Institute, said it's important for people to know what type of emergency care outpatient center they're going to and call ahead. Ask if they are licensed to handle emergency medical services.
- ●Retail Clinic
Retail Clinics are usually set up in supermarkets and chain pharmacies, such as Walgreens and CVS, to provide people with limited testing and medical care. Insurance companies do not necessarily pay retail clinic bills, and bills from retail clinics are not covered by the new law.
- ●birth center, nursing home or addiction treatment center
Hoadley pointed out that the provisions of the law for these institutions are relatively vague, and the key lies in whether it is a unit of a hospital that has signed a contract with an insurance company. If it is not a hospital affiliated unit, it may not be covered by the new law.
- ●Ambulance
According to the April 2020 Statistical Report of the Journal of Health Affairs, more than half of patients who are clients of well-known health insurance companies in the country received ambulance-related accident medical bills from 2013 to 2017. For a single bill, the amount is usually about $450.
Hoadley pointed out that some state or local governments prohibit ambulances from contracting directly with insurance companies, so ambulances used by people to seek medical care are provided through police departments, fire departments or other government agencies. The New York Times previously reported that the ambulance billing mechanism was so intricate that it was not included in the No Surprises Billing Act.
However, at least ten states in the United States have state laws that provide some protection for people using ambulances from unexpected bills, including Colorado, Delaware, Florida, Illinois, Maine, and Maryland, New York, Ohio, Vermont and West Virginia.
Thankfully, the No Surprises Billing Act provides protection from accidental billing for the use of air ambulance, both planes and helicopters, while the cost of air ambulance is included, the report said. It may cost tens of thousands of dollars.
"Consumer Reports" pointed out that people who use the medical services in the insurance company's system may still receive unexpected bills. If they receive unexpected medical bills, consumers can take measures to cope with the following:
★Avoid automatic payments
Karen Pollitz, a public health expert at the Kaiser Family Foundation, said the first step consumers can do is to contact the insurance company and ask if the hospital has issued a bill, and if the bill has not been issued, alert the insurance company and ask the hospital to send the bill directly to the insurance company. After the insurance company receives the bill, it will send the consumers Insurance Benefit Statement (Explanation of Benefits, EOB), which explains the details of the service charges in and out of the system.
If the amount of unpaid bills is still beyond the capacity, the consumers can ask the insurance company to provide a list of charges, so as to check whether there are double charges, or if the service is not used but was charged, and if there is a problem, report it to the insurance company or the hospital for processing. .
The Patient Advocate Foundation, a nonprofit that helps people deal with sky-high medical bills, estimates that nearly half of all medical bills contain major errors.
Consumers can also go to the medical information website healthcare bluebook.org to check the average cost of the same medical items in their ZIP code, so that they not only can have a more specific concept of the amount of the bill received, but also to help negotiate with the insurance company.
★Appeal to the federal government
The "No Surprises Bills Act" has a national consumer reporting system for medical bills, allowing the public to fill out a complaint form online, or call the toll-free number 800-985-3059 to report. When reporting, be careful to prepare all the information first. However, the whistleblower system does not have the power to help people negotiate unexpected bill amounts and can only allow bill charges to be waived or reduced under federal law.
★Appeal to the state government
Thirty-one states currently have state laws to varying degrees that protect people from unexpected medical bills. People can also file complaints with the state's Consumer Assistance Program.
★Uninsured public protection
Under the framework of the new law, medical institutions must provide a "good-faith estimate" for people who do not have medical insurance to explain the charges for medical services. If a person sees a doctor and receives a final bill that exceeds the estimate by $400, they can file a complaint with the Centers for Medicare and Medicaid Services. After a report is filed, the medical institution shall not send the bill to the collection agency for processing, nor shall it impose late fees until the dispute is resolved.
★ Seek free assistance
The "Patient Rights Foundation" website provides free services to the public, and the public can also call toll-free 800-532-5274 for inquiries. The Internet section "Ending Surprise Medical Bills" established by the Federal Medical Service Center provides detailed explanations of the consumer rights protection in the "No Surprises Bills Act", website: https://www.cms .gov/nosurprises.
(Source: World News Network)
This website has a free subscription function, please enter your email address and name (any nickname) in the upper right corner of the page. After subscribing, you can receive timely updates of the website. I hope that new and old readers will actively subscribe , so that we have the opportunity to provide you with better services
Please click: Home (wechineseus.com) for more news and content on this website
Follow The Chinese Media's Twitter account: https://twitter.com/wechineseinus
Follow The Chinese Media's Facebook account: https://www.facebook.com/wechineseinamerica/